Neurobehavioral Program
Timberlyn Heights provides neuro-rehabilitative services to individuals with acquired brain injury, traumatic brain injury, and/or a number of other neurological/organic conditions. The specialized services available in Timberlyn’s Neurobehavioral Rehabilitation program include neurological, neuro-rehabilitative, and neuro-psychiatric services, as well as intensive behavioral management and treatment services necessary to promote recovery, improved quality of life, and, if possible, transfer to a less restrictive, community-based setting.
MISSION:
The mission of the neuro-rehabilitative program is to provide quality rehabilitative services that result in the best possible outcomes to individuals who experience acquired brain injuries, neuro-psychiatric disorders, and other neurologic and behavioral disorders. More specifically, the program is designed to meet the needs and objectives of each individual served through comprehensive interdisciplinary treatment team services. Generally, this goal is driven by the pursuit of the following:
- Acquisition of functional skills in all critical rehabilitative domains
- Stabilization and improvement in social, emotional, and behavioral repertoires
- Optimal independent functioning in the least restrictive setting
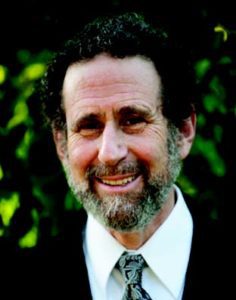
Dr. Lieff
Graduated from Yale College with a B.A. in mathematics, and Harvard Medical School with an M.D. He is a practicing psychiatrist, with specialties in geriatric psychiatry and neuropsychiatry. He was a pioneer in geriatric psychiatry, building some of the first geriatric medical/psychiatry hospital units, and the largest geriatric treatment network in New England, which he directed for twenty years. He is a specialist in the interface of psychiatry, neurology, and medicine.
Dr. Lieff is a past-president of the American Association for Geriatric Psychiatry (AAGP), the national subspecialty association. As president, he helped found the American Journal of Geriatric Psychiatry. He was the editor of the AAGP Newsletter for seven years and a consulting editor of the American Journal of Geriatric Psychiatry for 10 years. He helped found the Geriatric Psychiatry Committee and the High Technology Committee for the Massachusetts Psychiatric Society. He has been a member of several APA committees and chaired their Committee on Telemedicine.
Program Model and Structure:
The structure of the program is based upon individual residents/patients and their respective projected discharge settings (e.g., group home, long-term care, home with family, etc.). Program ‘discharge tracks’ are developed with the intent of approximating and/or preparing residents/patients for the characteristics and demands of the discharge setting, as much as practically feasible. Upon a referral, an evaluation is completed to provide the necessary information to determine that Timberlyn Heights is an appropriate placement. If appropriate, a proposed plan of care is developed and submitted for funding approval, followed by admission. After and during an initial assessment period, each resident’s care plan and program includes goals and objectives to accommodate individual strengths and challenges. These goals address the status of each resident’s cognitive, communication, physical, medical, behavioral, social, vocational, and other domains – with specific priority given to those skills critical to admission and success in the projected discharge setting/site. Services are offered through a variety of therapeutic contexts including 1:1, small group, and community oriented situations in a variety of relevant settings including unit-based, rehabilitation, and community settings.
The focus on each resident’s/patient’s program begins at the referral-admission stage, with a focus on the collaborative identification (i.e., by contributing stakeholders) of a projected discharge setting, if not a specific site. Once the discharge setting/site has been determined, the goal of assessment procedures is to evaluate the degree to which the resident’s/patient’s functional repertoire differs from the repertoire necessary to enter and function in the discharge setting – i.e., to identify the obstacles to successful discharge.
Care planning is then designed based upon discharge obstacles by identifying and prioritizing goals and objectives toward ameliorating these obstacles through various intervention and programming efforts which may include, but not be limited to:
- Physical Therapy
- Occupational Therapy
- Speech/Language Therapy
- Nursing & Medical Treatment
- Behavioral Interventions
- Psychiatric Interventions
- Neuropsychology
- Psychology & Counseling
- Vocational Services
- Therapeutic Recreation
- Education
- Applied Behavioral Analysis
- Cognitive Skills
- Life Skills
- Vocational Skills
- Leisure and Recreational Skills
- Communication Skills
- Social Skills
- Self-Management Skills
- Physical Functioning
- Medical Stability
- Wound Care
- Tracheotomy Care
- Other Nursing Care
Staffing and Training:
Timberlyn Heights’ staffing is as follows:
Professional Staffing
Program Director
Social Worker/Case Manager
RN/LPN, 24/7 coverage
Therapeutic Recreation
COTA or equivalent
Para-professionals
Mental Health Specialists (Neurobehavioral Rehab Specialists and Neurobehavioral Rehab Assistants), 24/7 coverage
Certified Nursing Assistants, 24/7 coverage
Beyond skills required for typical skilled nursing, staff training requirements include, but are not limited to, the following competencies:
- Program Mission and Philosophy
- Program Policies and procedures
- Safety-Care Behavioral Safety
- Psychiatric medication management
- Understanding diagnoses and symptoms
- Job descriptions
- Applied Behavioral Analysis
- Group leading/assisting skills
- Data Collection and documentation
- Discharge Planning
Ancillary Services
Physical Therapist
Occupational Therapist
Speech & Language Pathologist
Neuropsychologist
Neuropsychiatrist
Discharge Planning and Coordination
As noted earlier, every effort is made to identify a prospective discharge site prior to, or shortly after admission. Once identified, communication with the discharge site is maintained by the treatment team to continually update and adapt the resident’s/patient’s care plan to the pending site. As a resident/patient develops the skills necessary to approximate functioning in the prospective discharge site, more concrete planning takes place, eventually leading to successful transfer.

